Digital Stethoscope in the medical field
A virtual stethoscope is a modernized model of the conventional stethoscope that permits healthcare experts to electronically report, examine, and shop heart sounds and different body sounds. It gives several blessings over traditional stethoscopes, making it a treasured tool in the modern-day healthcare industry.
Digital stethoscope Usage
Using a digital stethoscope within reason is trustworthy. Here's a short step-by using-step manual:
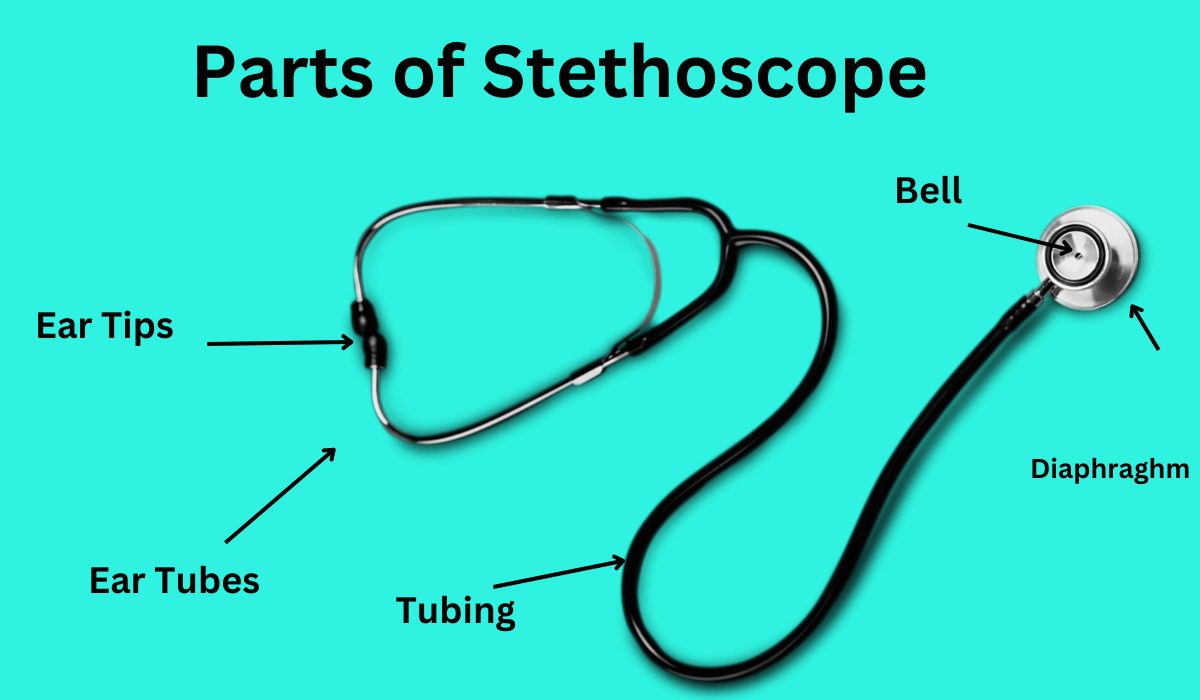
1. Place the earpieces to your ears and modify the quantity to a stage this is comfortable for you.
2. Connect the stethoscope to the tool by way of plugging it into the headphone jack or Bluetooth.
3. Turn on the tool and choose the mode you want to use, along with normal, amplified, or heart murmur.
4. Place the chestpiece at the affected person's chest, making sure that it is placed over the desired place.
5. Gently press down, permitting the coronary heart sounds to be transmitted through the chestpiece.
6. Listen to the heart sounds and another frame sounds via the earpieces.
7. If recording is essential, choose the document button and start taking pictures the sounds.
8. To forestall recording, press the stop button or turn off the device.
9. Analyze the recording, if necessary, the usage of the built-in software program or external software program.
10. Store the recording for your affected person's statistics for future reference.

Different digital stethoscope fashions come with varying features to beautify their overall performance and value. Here are some of the maximum not unusual capabilities:
1. Noise cancellation: This feature filters out history noise, making it less complicated to hear the heart sounds without a doubt.
2. Amplification: Some virtual stethoscopes have amplification competencies, allowing users to increase faint sounds.
3. Storage talents: Many virtual stethoscopes have integrated memory or the capability to connect to outside devices for storing recordings. This lets healthcare experts review heart sounds at a later time or percentage them with other healthcare specialists.
4. Connectivity: Some virtual stethoscopes are Bluetooth-enabled, allowing clients to wirelessly be a part of them to their smartphones or drugs for recording and playback. 5. Connectivity: Some virtual stethoscopes are nicely right with telemedicine structures, allowing healthcare experts to remotely listen to coronary heart sounds in real-time.
6. Software integration: Some digital stethoscopes have software integration competencies, allowing customers to research and export recordings to digital health document structures.
There are numerous key blessings that digital stethoscopes offer over conventional stethoscopes:
1. Increased accuracy and overall performance: Digital stethoscopes allow for more accurate detection of heart sounds and other body sounds, mainly to step forward affected person results.
2. Digital storage: The capability to shop recordings digitally eliminates the want for bodily paperwork, making it less complicated to get admission to and proportion affected person statistics.
3. Telehealth capabilities: Telehealth platforms enable healthcare professionals to remotely pay attention to coronary heart sounds, saving time and facilitating remote consultations.
4.Data evaluation: Digital stethoscopes provide advanced software program integration talents that allow customers to research recordings, generate opinions, and song developments.
Overall, digital stethoscopes provide numerous benefits over conventional stethoscopes, improving the quality of healthcare furnished.
With their superior abilities, stepped forward accuracy, and connectivity alternatives, digital stethoscopes are rapidly becoming the preferred desire for healthcare professionals.